Managing Pelvic Girdle Pain (PGP) in Pregnancy
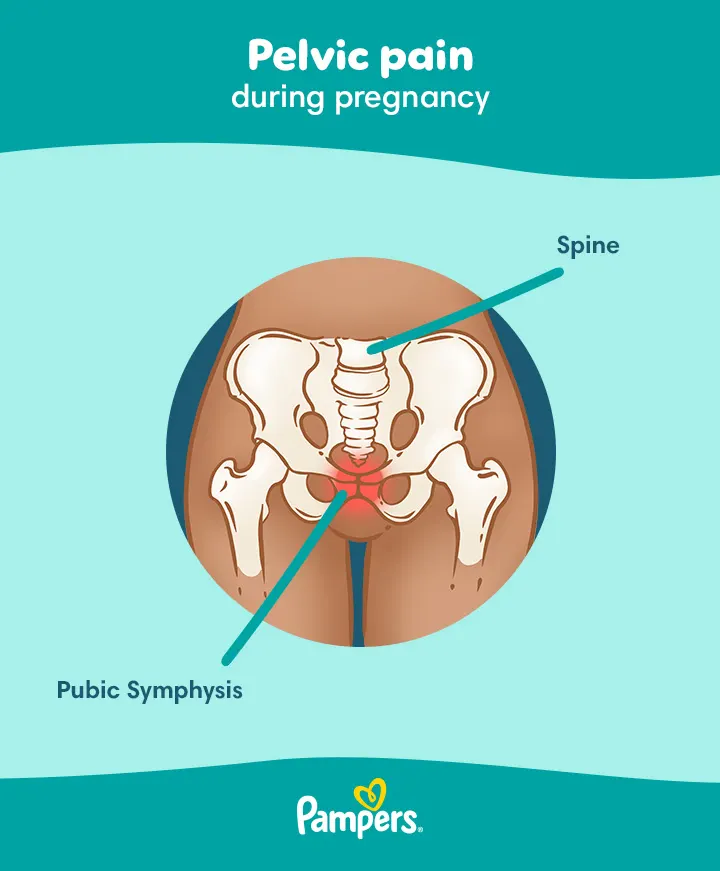
Pregnancy-related pelvic girdle pain (PGP), also known as symphysis pubis dysfunction (SPD), is a condition during pregnancy where the joints of your pelvis become more flexible due to hormonal changes preparing your body for birth. This increased flexibility may cause discomfort or pain in the pelvic area, which might affect your mobility.
While pelvic girdle pain may be challenging, the positive news is that there are ways to manage and relieve the discomfort during pregnant, and usually symptoms will ease or disappear entirely after your baby arrives.
Explore this guide to understand the causes, symptoms and treatment options for pelvic girdle pain during pregnancy.
What Is Pelvic Girdle Pain (PGP) in Pregnancy?
Pelvic girdle pain affects around 45% of pregnant people and 25% of people after birth to some degree. This condition arises when the joints in the pelvis, such as the pubic symphysis joint, become more mobile, often due to natural hormonal changes during pregnancy.
During pregnancy, your body produces a hormone called relaxin, which increases the flexibility of the ligaments supporting the pelvic joints. This added flexibility is essential as it allows the pelvis to widen in preparation for birth. However, in some cases, this increased laxity may lead to pelvic girdle pain during pregnancy, causing discomfort and affecting mobility. Fortunately, this pain often eases significantly after your baby is born.
Be sure to contact your midwife or GP if you experience any pelvic pain during pregnancy, as the cause of your discomfort may not be pelvic girdle pain. Your doctor can assess your symptoms, diagnose PGP and rule out other potential causes, such as an ectopic pregnancy, urinary tract infection, or pelvic inflammatory disease.
Pelvic Girdle Pain Symptoms in Pregnancy
Pelvic girdle pain may vary in intensity, ranging from mild discomfort to severe pain that might make daily activities challenging. Some people find that PGP makes it difficult to walk or perform regular movements. Here are some common symptoms:
If pelvic girdle pain becomes severe and limits movement to the extent that walking becomes difficult, it’s best to seek guidance from your midwife or GP.
Factors that may worsen PGP include:
Remember, pelvic girdle pain symptoms are usually manageable and most people find that discomfort eases after giving birth.
Pregnancy Weight Gain Calculator
Fill out your details:
Pelvic Girdle Pain Treatment
If you’re experiencing pelvic girdle pain during pregnancy, several treatment options may help bring relief. A combination of gentle exercises for pelvic girdle pain and targeted support may often make a significant difference.
To start, consulting a physiotherapist is advisable, as they can diagnose your specific pelvic girdle pain symptoms and recommend safe and effective treatments.
Common approaches include:
While pelvic girdle pain might affect mobility, consistent treatment may help improve comfort, allowing you to stay active and manage symptoms more effectively throughout pregnancy.
How to Relieve Pelvic Girdle Pain During Pregnancy
Managing pelvic girdle pain often involves a mix of rest, pacing yourself and targeted relief techniques:
Using these methods may help provide pelvic girdle pain relief and support your mobility throughout pregnancy.
How Can You Prevent Symphysis Pubis Dysfunction
While it may not always be possible to completely prevent pelvic girdle pain during pregnancy, certain exercises and lifestyle adjustments may help manage your symptoms or reduce pain. Research suggests that approximately 45% of pregnant people experience PGP, but the good news is that 93% see an improvement immediately after giving birth, likely due to the baby’s weight no longer placing stress on the pelvic joints.
It’s important to remember that pelvic girdle pain may take time to fully resolve, so allowing your body to recover after both pregnancy and birth is essential.
Pelvic Pain by Trimester
Pelvic girdle pain may appear at any point during pregnancy, though it most often begins between the second trimester (14 weeks) and the third trimester (30 weeks) and varies widely in its onset and severity. For example, for some people, Pelvic girdle pain symptoms may begin early as the body’s hormones start to affect the pelvic area, while others may only experience discomfort later in pregnancy as the weight and position of the baby place increased strain on the pelvis.
Regardless of when it begins, consistent management, such as engaging in gentle exercises for pelvic girdle pain, maintaining good posture and resting frequently, may help alleviate discomfort. If pelvic girdle pain symptoms become severe or interfere with daily activities, it’s best to consult a doctor, midwife or physiotherapist who specialises in pregnancy care for tailored guidance.
FAQS AT A GLANCE
To relieve pelvic girdle pain, your midwife or GP might recommend things like:
- exercises to strengthen your core muscles
- rest
- massage
- pain relief medications.
Bottom Line
Although pelvic girdle pain may cause discomfort during pregnancy, keep in mind that relief is often possible through treatments recommended by your doctor, midwife, or physiotherapist. And remember, the pain often eases after your little one is born, as the strain on the pelvis reduces naturally.
Pregnancy can bring its fair share of aches and pains, but many find that it’s all worthwhile once you're holding your newborn baby. For extra support, consider downloading the Pampers Club app, app if you haven’t already, which allows you to build up loyalty points and save on each purchase of Pampers nappies, nappy pants and baby wipes.
- NHS. 'Pelvic Girdle Pain'.
- NHS. 'Pelvic pain while pregnant (SPD)'.
- Pelvic Partnership. 'Do I Have PGP?'
- PubMed Central (PMC). 'The Pain May Radiate in Pregnancy'.
- Royal College of Obstetricians and Gynaecologists (RCOG). 'Pelvic Girdle Pain and Pregnancy'.
- South Tees Hospitals NHS Foundation Trust. 'Pelvic Girdle Pain in Pregnancy'.
Read more about Pregnancy
Related Articles
Join Pampers Club and get: