Jaundice in Newborns: Cause & Treatment
Have you noticed a yellowish tint to your baby’s skin or the whites of their eyes? It’s understandable to feel a bit worried – but know that newborn jaundice is very common, and in most cases, it’s completely harmless. Often, it’s simply a sign that your baby’s body is adjusting in the early days after birth.
Here’s a quick overview of what to expect:
In this guide, we’ll walk you through everything you need to know about jaundice in newborns – from the different types and causes to how it’s treated and when to seek medical advice.
What Is Jaundice?
Jaundice is a common condition in newborns where a baby’s skin and the whites of their eyes take on a yellowish tone. This happens when there’s a build-up of bilirubin in the blood. Bilirubin is a yellow pigment that forms when red blood cells break down. In the early days after birth, your baby’s liver may not be mature enough to remove bilirubin efficiently, which can cause it to accumulate.
You might be wondering, ‘How common is jaundice in newborns?’ The answer is – very. Around 60% of full-term babies and up to 80% of premature babies experience some degree of jaundice in their first week.
In many cases, jaundice appears a few days after birth and clears up on its own within two to three weeks. However, if it develops within the first 24 hours, worsens over time or lasts longer than expected, your baby’s doctor or midwife may wish to investigate further to rule out other causes.
Types of Newborn Jaundice
Several different types of jaundice can affect newborn babies. Some are entirely normal and tend to resolve on their own, while others may be linked to feeding patterns or underlying health concerns. Here’s what to be aware of:
Physiological jaundice.
This is the most common form and is considered a normal part of many babies’ early days. It usually appears around day 2 or 3 after birth, as your baby’s liver gradually matures and becomes more efficient at processing bilirubin. This type of jaundice typically clears up without treatment within about two weeks and is not usually a cause for concern.
Breastfeeding jaundice.
Occurring during the first week, breastfeeding jaundice may develop if your baby isn’t getting enough milk – often due to a delay in milk supply or challenges with latching or feeding. With additional feeding support and regular feeds, this type of jaundice usually improves and resolves over time.
Breast milk jaundice.
Distinct from breastfeeding jaundice, this type tends to appear a bit later, often after the first week, and may persist for several weeks. It’s thought to be linked to substances in breast milk that temporarily affect how bilirubin is processed. Breast milk jaundice is generally harmless, and there’s usually no need to stop breastfeeding.
Other causes.
Less commonly, jaundice in newborns may be linked to an underlying medical condition, such as an infection, enzyme deficiency, liver problem or a mismatch between the baby’s and parent's blood types (such as rhesus incompatibility). In these cases, your baby’s doctor or midwife will carry out further checks and recommend any treatment that may be needed.
Jaundice Signs and Symptoms
Symptoms of jaundice in your newborn might include:
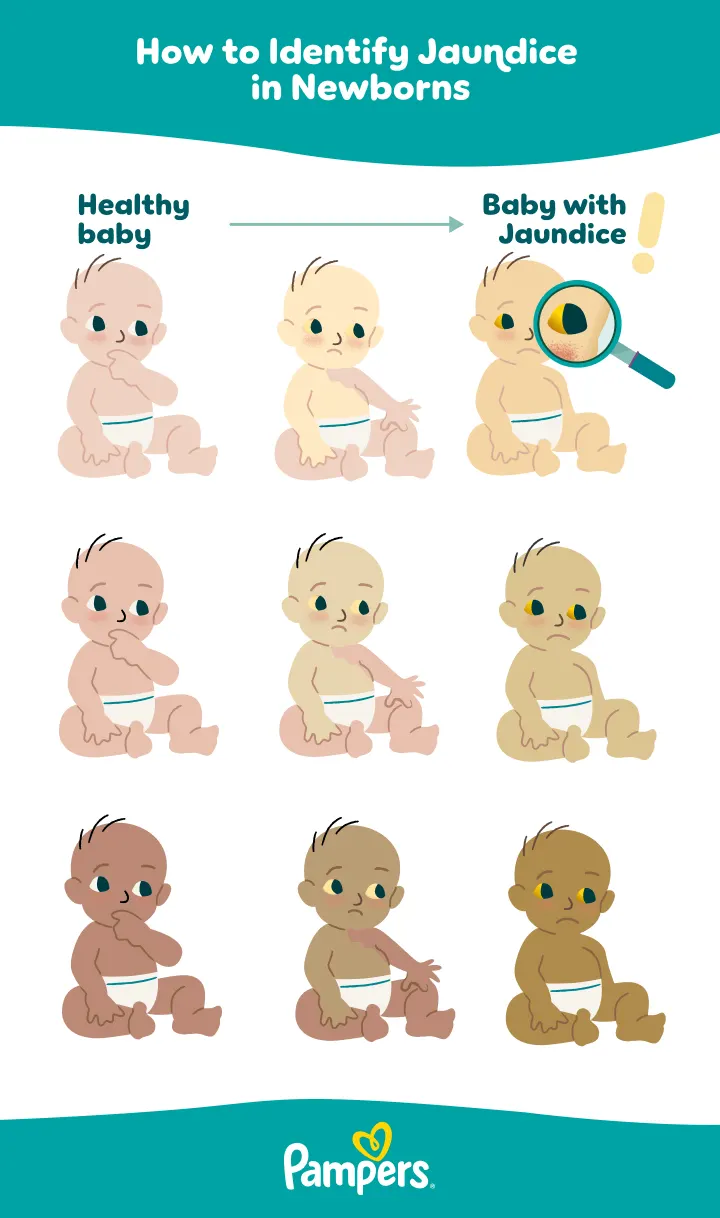
In babies with darker skin tones, the yellowing may be less noticeable. Instead of focusing solely on skin tone, check areas like the whites of your baby’s eyes, the inside of their mouth, and the palms of their hands or soles of their feet. These areas can give you a clearer clue.
Let your doctor or midwife know if you notice any of these signs.
Signs That Jaundice May Be Getting Worse
In most cases, jaundice will go away on its own after a few weeks, but if your baby shows any of the following symptoms – regardless of whether the jaundice is already being treated or monitored – your baby needs medical attention right away:
What Causes Jaundice in Newborn Babies?
Jaundice occurs when bilirubin (a yellow pigment created during the breakdown of red blood cells) accumulates faster than a baby’s immature liver can clear it. Several factors may increase the likelihood of elevated bilirubin in newborns.
Poor feeding/inadequate milk intake.
If a breastfed baby is not feeding frequently or taking enough milk (often in the first days), this can lead to a form of ‘breastfeeding jaundice’. Adequate feeding helps flush bilirubin via urine and stool.
Prematurity.
Babies born before term have even more immature livers and may break down red blood cells more rapidly, increasing the risk of jaundice.
Bruising or birth trauma.
If there is bruising (for example, after a forceps or ventouse delivery), red blood cells may break down more, contributing extra bilirubin.
Blood group incompatibility (ABO or Rh differences).
If mother and baby have different blood types (ABO incompatibility) or Rh factor mismatch, antibodies may lead to increased red blood cell destruction in the baby and raise bilirubin levels.
Red blood cell disorders.
Some genetic conditions (such as G6PD deficiency or other hemolytic disorders) cause red blood cells to break down more readily and can lead to higher bilirubin.
Infections.
Sepsis or other infections can impair the liver’s ability to process bilirubin and may contribute to jaundice.
Liver or biliary problems.
Rarely, structural or metabolic liver diseases (for example, biliary atresia) may underlie prolonged jaundice and require further evaluation.
Diagnosis
If your newborn shows signs of jaundice, your baby’s doctor will examine their skin, the whites of the eyes and possibly the gums. Your doctor may also check your baby’s urine and poo.
If jaundice is suspected, a medical device known as a bilirubinometer may be used to test the level of bilirubin in your baby’s blood. This works by shining a light onto your newborn’s skin and analysing the light that is reflected back.
A sample of your baby’s blood can also be tested for bilirubin, but this is usually only done if the jaundice has developed within the first 24 hours of birth, or if the bilirubinometer reading is very high.
The decision on whether any treatment is needed depends on the level of bilirubin.
More blood tests may be recommended if the jaundice lasts for more than two weeks, or if your baby needs treatment.
Newborn Jaundice Level Chart
In the UK, rather than a fixed ‘mg/dL chart by age’, NHS healthcare professionals use treatment threshold graphs from NICE to decide when phototherapy or other interventions are needed. These charts take into account:
Jaundice Treatment
In most cases, the jaundice will clear up by itself without treatment within a week or two. It’s important to keep breastfeeding or formula feeding regularly during this time because bilirubin leaves the body via your baby’s urine.
If the jaundice is making your little one sleepy and you think they may be feeding less as a result, ask your midwife or doctor for advice.
If your doctor determines that your baby needs treatment for jaundice, one of the following treatments may be recommended:
How Long Does Jaundice Typically Last?
It’s important to consult your healthcare provider about when your baby's condition is expected to return to normal. The duration of jaundice can vary based on its underlying cause and the treatment your baby is receiving.
Normal newborn jaundice typically resolves within a few weeks without special treatment. However, for reasons not fully understood, it may persist longer in breastfed babies.
If your baby’s jaundice needs treatment and/or it’s caused by another underlying condition, your doctor will be able to tell you how long it’s likely to last.
As your baby grows, it can be helpful to keep an eye on their development – especially after something like jaundice.
Try our Baby Growth Chart Calculator to track their weight, length and head size against UK growth standards.
Possible Complications Associated With Jaundice
In some cases, if left untreated, extremely high levels of bilirubin can affect the brain and result in a serious condition known as kernicterus. Prompt treatment is the best way to protect against complications like this.
Don’t worry, kernicterus is rare. In fact, it affects fewer than 1 in every 100,000 babies in the UK.
FAQS AT A GLANCE
Most cases of jaundice are mild and resolve on their own. However, if bilirubin levels become excessively high and are left untreated, jaundice can lead to serious complications. Always consult your baby's doctor or midwife if you notice worsening symptoms or persistent yellowing of the skin.
The Bottom Line
Jaundice is very common in newborn babies, and most often it’s the kind that will clear up on its own within a couple of weeks.
Remember that quick diagnosis and treatment can help ensure that the jaundice is well managed and doesn’t cause any problems for your baby. Soon, things will likely settle down, and you can get on with enjoying the newborn phase.
Turn your Pampers nappies and wipes into rewards. Download the Pampers Club app today and start earning with every change!
- NHS: Jaundice
- NHS: Jaundice in babies
- NHS: Jaundice in newborn babies
- NHS: Jaundice in newborns
- NHS: Jaundice in the newborn baby
- NHS: Neonatal Jaundice
- NHS: Neonatal – Jaundice in the newborn baby
- NHS: Neonatal Jaundice – NICE threshold
- NHS: Overview - Newborn jaundice
- NHS: Overview - Rhesus disease
- NICE: Jaundice in newborn babies under 28 days
Read more about Newborn Baby
Related Articles
Join Pampers Club and get: